Medical Treatment
Lumbar spinal canal stenosis
As shown in Fig. 2-1, the lumbar vertebrae have a vertebral foramen, which are connected vertically to form a canal called the spinal canal. The spinal cord is contained in this canal. The spinal cord is then surrounded by the following tissues. In front of the spinal cord, there is an intervertebral disc between the vertebrae, and behind the disc is a longitudinal ligament called the posterior longitudinal ligament. And behind the spinal cord, between the vertebral discs, is the yellow "yellow ligament". The spinal cord is surrounded by the vertebrae, intervertebral discs, posterior longitudinal ligament, and yellow ligament. When these protrude toward the center of the spinal canal due to deformation, herniation injury, or thickening, the spinal canal becomes narrower, putting pressure on the spinal cord causing spinal stenosis.
In other words, spinal stenosis is a narrowing of the spinal canal caused by vertebral deformity, lumbar herniation, lumbar spondylolisthesis, sclerosis of the lumbar spine or yellow ligament. This causes intermittent claudication, a condition in which after a short time of walking, the legs and hips become numb, painful, or sluggish, and the patient is unable to walk.
It is a common disease among people aged 60-79 years, and the number of those who answered "always" or "sometimes" accounts for 60% of the total number of patients. It is one of the most intractable diseases.
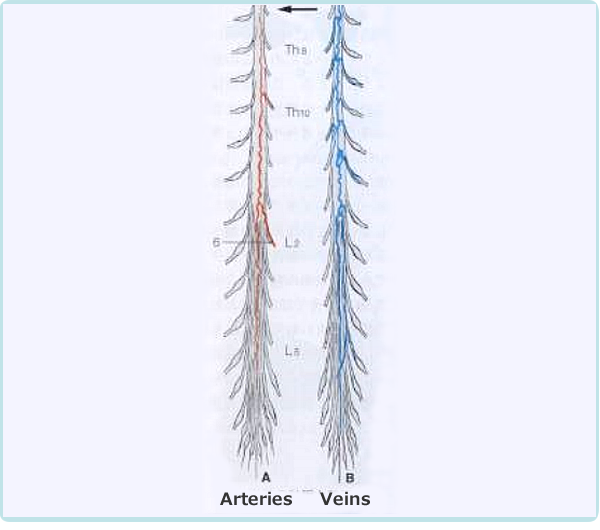
The mechanism of intermittent claudication is as follows. In scoliosis, the cauda equina nerve, which is located below the second lumbar vertebra. It resembles a horse's tail and is compressed by a deformed yellow ligament or vertebra causing pain and numbness in the lower extremities. The cauda equina nerve has longitudinally distributed blood vessels that supply oxygen and nutrients to the nerve root as shown in Figure 2-2.
As the lumen of the lumbar spinal canal narrows, the nutrient vessels of the caudal nerve are compressed and narrowed. When the lumbar spine kyphosis is strengthened by upper body loading (60% of body weight) during walking, the spinal canal is further narrowed and the pressure on the blood vessels becomes stronger. As a result, blood flow to the cauda equina nerve deteriorates, causing pain and numbness in the lower limbs, making walking difficult (intermittent claudication).
Thus, the mechanism of the pain, numbness, and burning sensation in the hip and lower limbs during walking is due to the blood flow disturbance caused by the compression of the blood vessels that nourish the spinal cord. New meridian therapy effectively improves numbness and pain during walking without the need for surgery. The mechanism of this effect is thought to be that it improves blood flow around the spinal canal and spinal blood vessels, reduction of edema due to inflammation of the tissues around the spinal canal, thereby improving the narrowing of the spinal canal. At the same time it repairs and expands the spinal blood vessels, thereby improving blood flow.
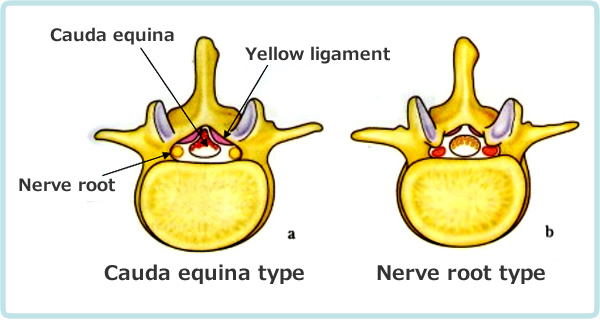
Adapted from Kikuchi: Journal of the Japan Orthopedic Association, 62: 571, 1988.
| Type | Cauda equina type | Nerve root type |
|---|---|---|
| Common symptom | Neurogenic intermittent claudication | |
| Subjective symptoms | Abnormal sensation (burning) in lower limbs, buttocks, and perineum | Pain in lower limbs and buttocks |
| Objective findings | Polyradiculopathy | Single-rooted disorder |
Table 2-1 compares the symptoms of the cauda equina type and the nerve root type. The cauda equina type is characterized by bilateral burning sensation due to thickening of the yellow ligament. The nerve root type is pain in the lower extremities and hip region due to unilateral nerve root compression caused by vertebral deformity or herniation. The common symptom is gait disturbance due to symptoms in the lower extremities and hip when walking. The nerve root type is easily cured, but spontaneous healing of the cauda equina type is difficult.
Treatment case 1.
65-year-old woman with spinal canal stenosis
- Chief complaint
- Numbness and pain in the right hip to lower limb when walking, walking disorder.
She had intermittent claudication for 8 years, and despite more than 100 block injections at a pain clinic, the pain did not get better. 2 years ago in January, she underwent surgery of the 3/4th, 4/5th disc in her lower back. 1 year ago in February, she underwent surgery of the 2/3rd, 3/4th disc in her lower back, and the pain got relieved. However, in December of the same year, the pain recurred, making it impossible to get up in the morning and causing difficulty walking. In December of the same year, she received a block injection. In January of this year, after 3 weeks of bed rest at home, she received sacral epidural block injection, intravenous injection, and hot pack, and her symptoms were relieved, but she still has symptoms of numbness and pain in her lower limbs when walking. - Occupational/History
- 23 years working in general office work; at age 45, had a morning back sprain. Occasional back pain led to orthopedic rehabilitation.
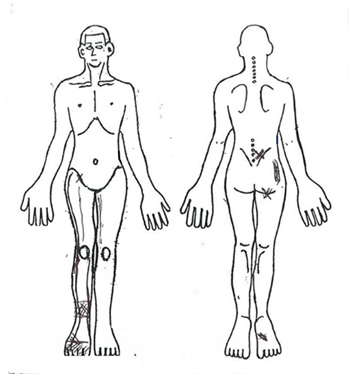
Figure 2-3. Symptoms in the hip and lower extremities. 
Figure 2-4. Hernia of L3/4 and L4/5 by MRI - Treatment course
- Symptom: Pain in the lower leg at the bile meridian (meridian on the outer side of the lower limb) during right oblique forward bending of the lumbar region.
- First treatment (Tx),
- the pain in the bile meridian almost disappeared and walking became smooth. She was also able to extend her right leg.
- 2 Tx
- the pain in the bile meridian disappeared.
- 15 Tx
- the patient's gait was almost completely improved.
- 19 Tx
- the pain in the right lower leg improved from VAS 10/10 points to 0/10 points. Pain in the right thigh improved from 10/10 points to 3/10 points, and gait improved from 10/10 points to 0/10 points.
- Summary
- This is a case in which symptoms of spinal canal stenosis, which had recurred and did not improve with intermittent claudication even after two surgeries, disappeared with the new meridian therapy. Thus, the new meridian therapy is remarkably effective for spinal canal stenosis.
Treatment case 2.
70-year-old woman with L4/5 spinal canal stenosis, lumbar spondylolisthesis
Back pain started 10 years ago. She perceives pain in half-standing posture, etc. Two years ago, back pain worsened and she visited an orthopedics. MRI showed age-appropriate diagnosis, and X-p showed slip at L4/5. She took painkillers and had injections, but they had no effect. Her husband passed away at the end of the year, and she was overwhelmed by the cleanup work.
When she went up and down stairs more than 7 steps, she felt pain in her left low back. 20 minutes uphill, she felt pain in her left low back. She felt pain in 2 to 3-minute half-standing. Crouching posture is normal, and she can sit in a chair for 1 hour.
-
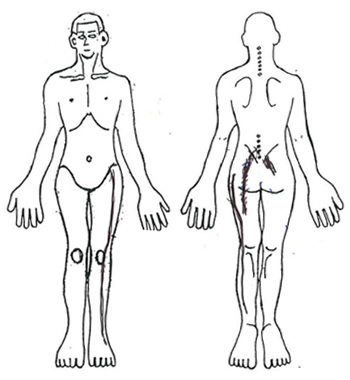
Figure 2-5. Findings in the lower back and lower extremities 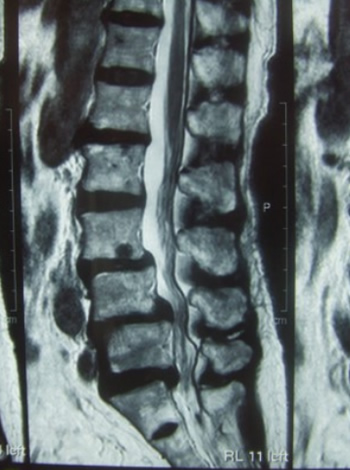
Figure 2-6. Anterior slip at L3 and L4, posterior slip at L5, and spinal canal stenosis at L3/4, L4/5, and L5/S1. 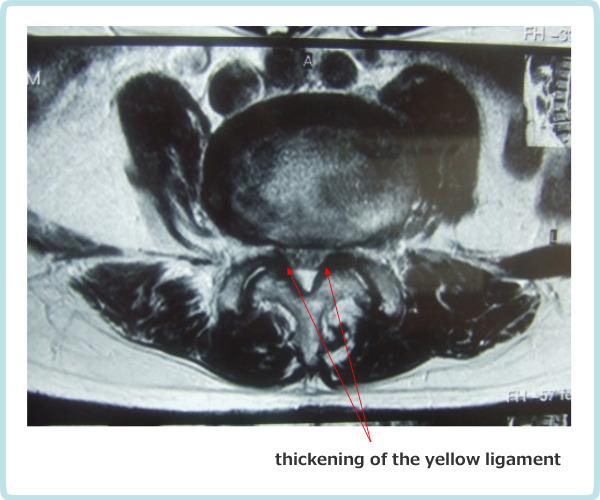
Figure 2-7. Compression of the cauda equina nerve from the dorsolateral aspect due to narrowing of the L3.4 intervertebral foramen and thickening of the yellow ligament 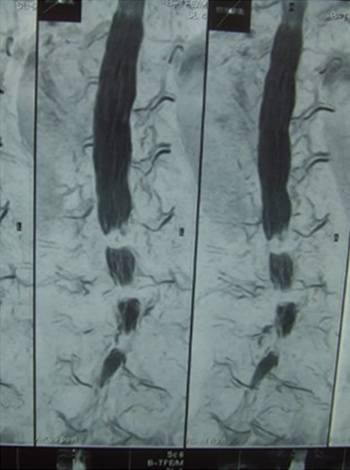
Figure 2-8. Stenosis of L3/4, L4/5, and L5/S1 - Treatment course
-
- Just after 1stTx
- L4 pain in the morning.
- 1Tx
- Pain when lying on the side.
- 3 Tx
- she changed her soft bed to a futon.
- 6 Tx
- on the 10th day of using the futon. Morning movement of her hips was light.
- 15 Tx
- the pain was relieved, but the dull ache remained.
- 21 to 26 Tx
- her back pain improved and she went on an overseas trip.
- 35 Tx
- she has a board on her bed. Now, her lower back stretches in the morning.
- 65 Tx
- morning lower back pain is better.
- 71 Tx
- ain on the right side of her lower back. She thought it was caused by high heels, so she stopped wearing them.
- 72 Tx
- she changed her shoes and her right hip pain when walking decreased.
- 75 Tx
- her back pain decreased and morning back pain became less severe. Treatment was terminated as an abbreviated cure.
- Summary
- Intractable spinal canal stenosis was improved by adding ergonomic measures to new meridian therapy without surgery. Thus, the new meridian therapy is effective even in cases with spondylolisthesis. The patient was monitored for a long period of time afterwards, and the symptoms have not recurred and the patient is doing well.
Treatment outcome of spinal canal stenosis in 18 subjects
Of the 41 subjects who visited our clinic for suspected spinal canal stenosis between 2005 and 2015, we analyzed 18 subjects who satisfied the 4 conditions of the Japanese Orthopaedic Association's lumbar spinal canal stenosis treatment guidelines, were treated at least 5 times, and had complete data.
Treatment consisted of connecting, reinforcing, and overcoming treatment of the bladder and kidney meridians to the stenosis site. 1 treatment session lasted about 15 minutes.
Treatment evaluation was performed by walking distance: one step was estimated as 50 cm and one hour walking distance as 4 km.
Four conditions of the subject's diagnostic criteria: The above guidelines for the lumbar spinal canal stenosis were followed.
1) Pain or numbness in the lower limbs from the hip to the lower limbs.
2) Pain and numbness in the lower limbs from the hip to the lower limbs appear or are aggravated by standing or walking, and are alleviated by bending forward or sitting.
3) Low back pain that is aggravated by walking should be ruled out if it is isolated.
4) MRI or other imaging studies confirm degenerative stenosis of the spinal canal or intervertebral foramen and can explain the clinical findings.
| Gender | 6 male (33.4%) | |
| 12 females (66.7%) | ||
| Mean | SD | |
| Age (yrs.) | 68.7 | 8.9 |
| Observation period (week) | 15.7 | 12.4 |
| Disease type | Cauda equina type (%) | Nerve root type (%) |
|---|---|---|
| N (%) | 8(44.4) | 10(55.6) |
| Male/female | 2/6 | 4/6 |
| Mean±SD | Mean±SD | |
| Age | 70.3±8.7 | 67.5±9.3 |
| Walk distance (m) at first visit | 432.9±275.7 | 237.8±297.3 |
| Disease type | Cauda equina type | Nerve root type |
|---|---|---|
| N | 8 | 10 |
| Mean±SD | Mean±SD | |
| Number of treatments (times) | 42.8 ± 42.8 ns | 22.5 ± 17.8 |
| Walking distance at first visit (m) | 432.9 ± 275.7 ns | 237.8 ± 297.3 |
| Walking distance at final visit (m) | 2775.0 ± 2468.7ns | 1816.7 ± 1078.6 |
| Greatly improved (%) | 7(87.5) | 8(80.0) |
| Much improved (%) | 2(20.0) | |
| Slightly improved (%) | ||
| No change (%) | 1(12.5) |
ns p>0.05, no significant difference in number of treatments. (Welch's t-test (number of treatments, walk at last visit/ t-test (walk at first visit))
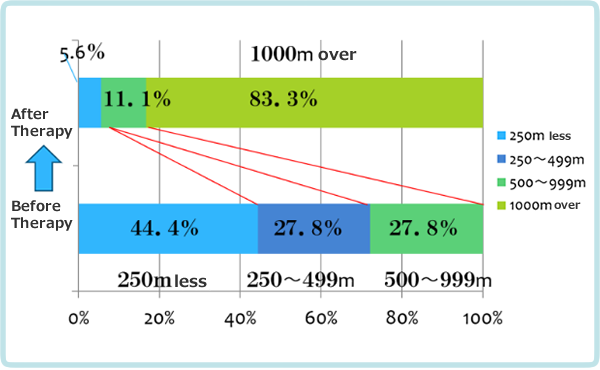
Results
The average number of new meridian therapy was 31.5. The average walkable distance was 324.5 m at the first visit and improved to 2242.6 m at the last visit, a seven-fold improvement. Improvement to 1,000 m or more without pain or numbness was defined as " greatly improved," 500 m to 1,000 m as "moderately improved," 250 m to 500 m as "little improved," and less than that or no improvement as "no change.
83.3% of the patients reported 'very much improved' and 94.4% reported 'much improved' or more (see Figure 2-9). The new meridian therapy is highly effective in improving gait, suggesting that it improves inflammation of the cauda equina nerve, edema of the spinal canal, and blood flow in the spinal vessels.