Medical Treatment
Chemical sensitivity
Yuwa Clinic offers treatment for chemical sensitivity. First, we will discuss how chemical sensitivity has been recognized historically. Then, we discuss the treatment of chemical sensitivity.
Historical course of the discovery of chemical sensitivity
In 1947, Dr Theron Randolph, an American physician, proposed the "possibility of hypersensitivity reactions caused by exposure to chemicals". Dr Randolph found that the first patients' symptoms, such as headaches that changed with the wind direction, were caused by chemicals in the air pollution. He then named the condition Chemical Sensitivity. At the time, however, his ideas were not generally accepted.
Later, as incidents of 'chemical sensitivity', such as Sick Building Syndrome, caused by the spread of chemicals became more frequent, Dr Randolph's ideas became more accepted.
Then, succeeding Dr Randolph, the concept of Multiple Chemical Sensitivity (MCS) was proposed by Dr Mark Cullen in the 1980s. This was described as 'a condition in which a person has a hypersensitivity reaction to very small amounts of chemicals after chronic or massive exposure to chemicals, with a wide range of symptoms'. Since then, research has been conducted mainly by medical researchers known as 'clinical environmentalists' who advocate a similar concept.
The incident that triggered this was a 1981-1982 incident at the Environmental Protection Agency (EPA) in the USA when carpets were being replaced and volatiles from an adhesive called 4-phenylcyclohexane were released into the air at concentrations of 13-15 ppb, causing 124 of the 2000 employees to developed the disease, two retired and 17 were subsequently unable to return to work due to hypersensitivity. After the onset of the disease, even very low concentrations of 1 ppb can cause symptoms. This incident caused the very chemical sensitivity case. Such hypersensitivity cases also occurred in hospitals and buildings in Nova Scotia, Canada, and a 24-hour open facility for the problem was opened at Dalhousie University under government control (measures to cause air circulation). (Bibliography Satoshi Ishikawa and Mikio Miyata: Chemical Sensitivity, from Kamogawa Publishing, 1999)
Dr Randolph founded the Society for Clinical Environmental Studies in 1965 as an organization to promote his theories based on the symptoms of patients with what are known as multiple chemical sensitivities (MCS). It is now the American Academy of Clinical Environmental Studies.
And in Japan, the Japanese Society of Clinical Ecology was established in April 1992 by Ishikawa et al. to promote research. In Japan, the Kitasato Research Institute Hospital introduced the concept of MCS, and diagnostic and therapeutic methods have been studied as 'chemical hypersensitivity'. The Kitasato Institute Hospital Centre for Clinical Environmental Medicine was subsequently established.
Note: The Japanese Society of Clinical Ecology: established to promote the development of research on the relationship between the environment and diseases, and to prevent and treat diseases in cooperation with relevant institutions. The conference covers poisoning, allergy, endocrinology and autonomic nervous system, with the subject of research on the interface between environmental issues and clinical medicine. Regarding the environment, the conference aims to cover a wide range of chemical, physical and biological environments.
Ishikawa et al. point out that the true nature of chemical hypersensitivity is "parasympathetic predominance" as a pathology of the autonomic nervous system, and this is a major clue.
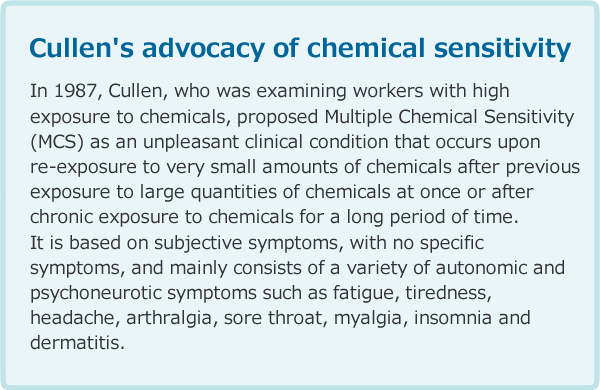
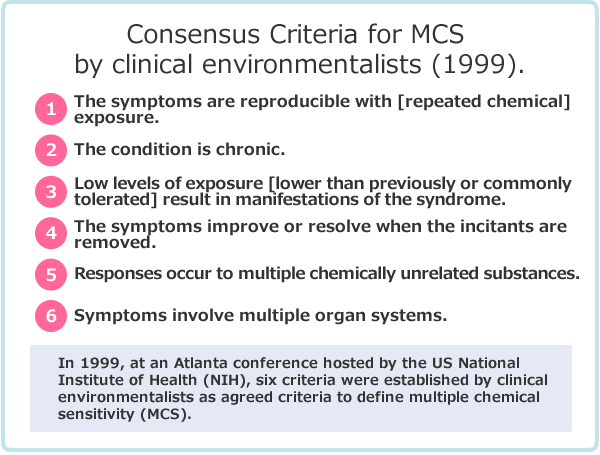
Table 2 shows a widely used definition of multiple chemical hypersensitivity proposed by the clinical environmentalists at the Atlanta conference organized by the National Institutes of Health in 1999. Chemical hypersensitivity is characterized by 1) reactions occurring even at low concentrations, like an immune response (hypersensitivity training effect), 2) reactions to a wide variety of unrelated chemicals, and 3) symptoms are not organ specific (no organ specificity) and many different organs are involved.
National response to chemical sensitivity in Japan
Since 1 October 2009, the Ministry of Health, Labour and Welfare (MHLW) has registered chemical hypersensitivity on its list of diseases, allowing it to be included in medical records and medical fee statements (receipts).
Chemical hypersensitivity is registered in the Standard Disease Names Master and as T65.9 (toxic effects of substances of unknown detail) in the basic classification code, ICD-10, chemical hypersensitivity is covered by insurance medical treatment.
In addition, the Japan Pension Organization, which is under the supervision of the Ministry of Health, Labour and Welfare (MHLW), has recognized patients with chemical sensitivity as eligible for disability pensions since 2010. Patients at the Yuwa Clinic have also received disability pensions for hypersensitivity.
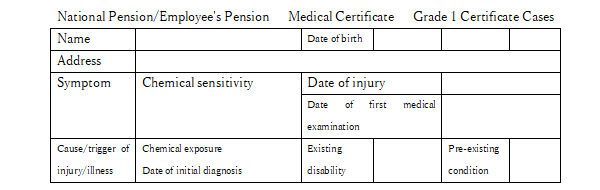
Table 3 shows examples of severe disability class 1 certifications as listed on the medical certificate form for chemical sensitivity issued by the Japan Pension Service. It is described as follows. Initial medical examination findings "From around February 2010, she reacted to synthetic detergents and other substances in the workplace and developed palpitations, dizziness, shortness of breath and other indefinite complaints. This was followed by symptoms such as difficulty walking due to numbness and weakness in the limbs and loss of appetite. Her symptoms gradually worsened and she was diagnosed with severe chemical hypersensitivity, a reaction to airborne chemicals."
The doctor's treatment description states. 'The patient has been seen in our clinic since May 2013 and has been treated with medication, but her symptoms did not improve. Treatment was guided by providing information on food and clothing with low chemical content, as it is important to reduce exposure to chemicals." This case shows that hypersensitivity can be extremely serious in severe cases.
Examples of treatment at the Yuwa Clinic
The Yuwa Clinic has been treating patients with chemical hypersensitivity since 2009. The first patient developed hypersensitivity due to chronic exposure to organic solvents at an environmental measurement institute when cleaning analysis instruments with residual organic solvents. She was also hypersensitive to deodorants at home. The hypersensitivity symptoms were cured after receiving occupational injury certification and treatment.
Since then, more cases of hypersensitivity have been treated. In a recent case study, three hypersensitivity patients from an environmental analysis workplace were treated and cured; the common features of the three cases were 1) all were women, 2) they reacted to very low concentrations of formaldehyde and other substances that do not cause poisoning, and 3) initially, they had sick building syndrome, a reaction to volatile substances in the workplace such as formaldehyde. 4) the symptoms involve multiple organ systems, although they vary from person to person; 5) symptoms decrease when leaving the workplace, but about 20-30% of hypersensitivity reactivity remains long-term, and the activated charcoal mask can not be taken off when going out. 6) Acupuncture (new meridian therapy) and Chinese herbal treatment to regulate the autonomic nervous system were effective in reducing symptoms in the three patients.
化学物質過敏症の機序
(Modified from Sensitivities National Academy Press 1992 Ashford diagram. (Ishikawa, T. et al. p66)
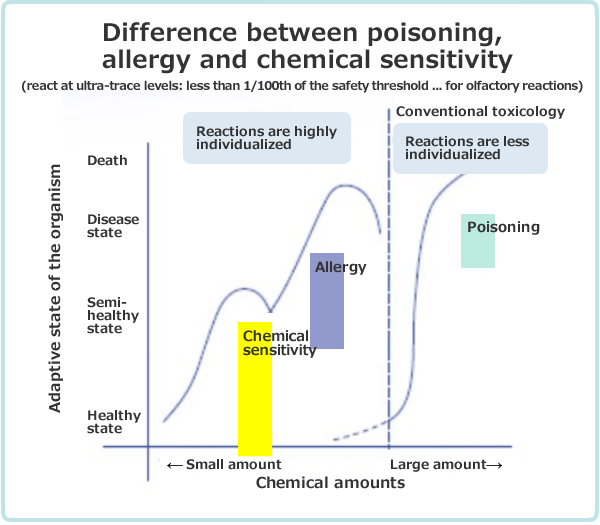
Figure 1 shows the differences in chemical load and response between conventional poisoning, allergy and chemical hypersensitivity, where the amount of chemical reacting decreases in the order of poisoning > allergy > chemical hypersensitivity, with chemical hypersensitivity reacting at very low levels, less than 1/100th of the safety threshold. This is a characteristic feature of hypersensitivity.
Conventional poisoning is symptomatic in roughly 100% of patients when the chemical increases. Minamata disease due to methyl mercury and sarin poisoning are good examples.
With allergies, even if a chemical substance is increased, not everyone will show symptoms; some people will become allergic and others will not, as their natural constitution is involved. However, in the case of allergies, the symptoms are clear, such as atopic dermatitis, asthma, allergies to the eyes and nose, and abnormalities such as high immunoglobulin IgE in blood tests are easily detected, so people around them can easily recognize them. In other words, it is important that the individual's reactivity is strongly affected. Some also have substance specificity, as in acquired immunity. However, in children's allergy, it is thought that an immune overstimulation state is occurring, as the child reacts to dozens of different foods instead of just a substance, such as dust mites. Allergic reactions can occur when the body is sensitized by a foreign substance (antigen) that has entered the organism and then reacts hypersensitively when it comes into contact with that foreign substance again. This reaction is called an antigen-antibody reaction. The Austrian paediatrician C. Pirquet first proposed the theory of allergy in 1906. (From the International Encyclopaedia Britannica)
The theory of allergy is based on the theory of Dr Abo et al. that the parasympathetic nervous system is linked to lymphocytes and that when parasympathetic dominance is reached, lymphocytes increase, resulting in a state of hyperimmunity.
This is believed to be the nature of allergy as hyperimmune. As a result, as the allergy progresses, the person reacts to even harmless substances. This indicates that a person originally has a system that reacts to several foreign substances. (The concept of innate immunity)
In chemical hypersensitivity, a person reacts to incredibly small amounts of chemicals, usually less than 1/100th of the safety threshold. In the USA, the leading chemical sensitivity country, it is estimated that around 15% of people show this symptom.
Neurological symptoms are common, medical tests are unlikely to reveal abnormalities, and it is often difficult for those around them to understand the symptoms. The problem with this hypersensitivity is the total load caused by the combined intake of chemicals. Severe cases have experienced three new houses. Many cases develop suddenly one day after repeatedly moving to a new house or a renovated house, first or second time. In some cases, the last new house was the final straw for the onset of chemical sensitivity. These illustrate the importance of the sum of the chemicals, i.e. the total load.
This concept of total load is the same as that of chronic poisoning. However, it differs from chronic poisoning in that "the amount of chemicals required for the onset of the disease is very small" and "once the disease has started, the person will then react to very small amounts of chemicals".
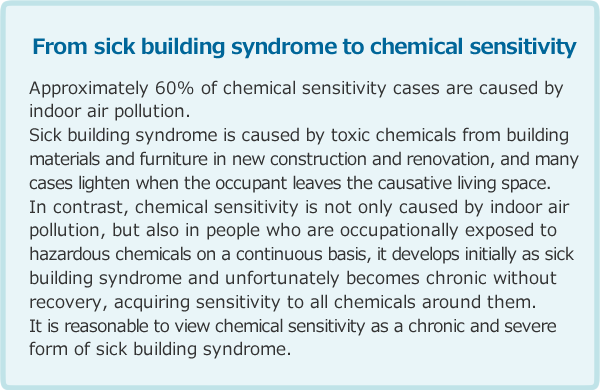
Table 4 shows the relationship between sick building syndrome and chemical sensitivity according to Ishikawa et al. Ishikawa et al. state that the sick building syndrome is a chronic form of chemical sensitivity. Our experience supports this.
What substances trigger hypersensitivity? Reaction of eliminating toxic substances
Previous research has indicated that formaldehyde, organophosphorous compounds, pesticides and insect repellents, and organic solvents such as toluene are the main triggers of hypersensitivity. More recently, synthetic air fresheners in fabric softeners, antiperspirants and synthetic fragrances have been added to the list of causes of hypersensitivity as 'fragrance hazards'.
It is clear from this that the chemicals that play a leading role in chemical hypersensitivity are mainly highly irritating substances, which are toxic and cause a burden on the organism. It is thought that these highly irritating and toxic compounds trigger chemical hypersensitivity and subsequently It is clear from this that the chemicals that play a leading role in chemical hypersensitivity are mainly highly irritating substances, which are toxic and cause a burden on the organism. It is thought that these highly irritating and toxic compounds trigger chemical hypersensitivity and subsequently lower the threshold so to react to relatively less toxic compounds.
It is believed that humans have acquired, in the course of evolution, an eliminating mechanism (parasympathetic mechanism) that avoids many phytotoxins and bacterial putrefactive poisons that they come into contact with in the environment. (Randolph M. Nessy & George. C. Williams, Why Disease Is, Shinyosha, 2009, Margie Prophet, Adapted Mind, New York: Oxford Uni. Press 1992)
Chemical hypersensitivity is thought to be a condition in which this defense mechanism against phytotoxins and other chemical toxins acquired by humans during evolution, i.e. the spontaneous eliminating response, is activated, remembered and reinforced by chronic exposure to irritating volatile gases such as formaldehyde, resulting in hypersensitivity, and subsequently the eliminating response is extended to less toxic substances as well.
In summary, the mechanism of hypersensitivity onset is as follows.
- 1
- Exposure to irritating volatiles → irritation of eyes, nose and airways → activation of the toxin elimination system acquired during evolution (parasympathetic nervous system) → tears, runny nose, sneezing, coughing, sputum, saliva, nausea and vomiting → avoidance behaviour from volatiles and escape.
- 2
- In the early stages, symptoms subside when people move away from exposure to irritating volatiles. (Stages of Sick Building Syndrome)
- 3
- If exposure to irritating volatile substances cannot be avoided, e.g. at work or in the house, and continues for several months (2-3 months), the parasympathetic toxicant elimination system is continuously enhanced, resulting in parasympathetic dominance → sensitization (long-term potentiation at the synapse) occurs. This leads to elimination reactions even to relatively less irritating substances. (Stage of multiple chemical hypersensitivity).
- 4
- Ishikawa et al. studied patients with chemical hypersensitivity and noted from pupil response tests that a significant number of people have 'parasympathetic dominance'. A chronic state of parasympathetic dominance = hyper-sensitivity of the toxin elimination system is thought to be the true nature of chemical hypersensitivity.
- 5
- There are individual differences in susceptibility to the toxin elimination system. It is stronger in females than in males. Ishikawa et al. suggest that this is because the sensitivity of the sensory system - e.g. the sense of smell - is more sensitive in females than in males, and because the instinct to preserve the species means that females are designed to flee dangerous environments first with their children. Animal studies have also demonstrated that females are more sensitive to chemicals.
The director of the US National Institute of Environmental Health Sciences, Dr Sansaman, states that women are generally more susceptible to the effects of environmental toxins.
Diagnosis
For the diagnosis of chemical hypersensitivity, it is important to interview the patient about the course of the disease.
1) Medical history
The most important part of the diagnosis is the medical history. This will almost always make the diagnosis, and R. McLellan in 1987 emphasized that the two absolute questions to ask in the diagnosis are 'what are you reacting to' and 'why did you become so hypersensitive'.
Taking time, you need to ask for a detailed history of chemical contact, including occupational and domestic history. A detailed chemical interview is necessary, especially as the total chemical load is related to the onset of the disease. The interview should include a detailed history of moving house, lifestyle, the amount of chemicals used in the living environment, frequency and duration of contact, and furthermore, the diet. In particular, they are asked in detail about new buildings, renovations, moving history, residential history, hobbies, etc. They are also asked about the presence or absence of air pollution in the dwelling.
2) Examinations
The following tests can be used as supplementary information
- a. Neurofunctional tests
- Pupil examination
When light enters the eye, the pupil contracts, and when it is darkened, the pupil widens. These pupils contract with the parasympathetic nervous system and enlarge with the sympathetic nervous system. Measuring the diameter of the pupil shows that in chemical sensitivity the diameter of the pupil is contracted compared to normal values for different age groups.
Accommodating test
In chemical hypersensitivity, the ciliary muscle is spasmed and the ability to accommodate is impaired. The patient's ability to regulate focusing is tested. If necessary, refer to an ophthalmologist for further examination.
Eye movement test
The eyeballs can smoothly follow a moving target in front of them. In chemical sensitivity, this tracking motion is reduced and the eye cannot follow the indicators in front of it as well as it should.
Center-of-gravity sway test
In chemical hypersensitivity, the equilibrium function is impaired due to a disturbance in central nervous system function. In the center-of-gravity sway test, the patient is placed on a plate and the trajectory of the center of gravity is recorded when the eyes are open and closed. - b. Pulmonary function tests
- Respiratory function is tested using a spirometer, a pulmonary function testing machine. Pulmonary function tests are performed in chemical hypersensitivity, as there is often a decrease in V25, which indicates peripheral airway obstruction.
Various medical certificates, etc.
If necessary, we can prepare a medical certificate for absence from work related to chemical sensitivity, a medical certificate for injury and illness benefits, a medical certificate for a disability pension for chemical sensitivity, a medical certificate for work-related accidents, etc.
Treatment
So far, we have treated chemical sensitivity and the symptoms of hypersensitivity have steadily improved. Some patients have even improved to the point where they are able to work.
Treatment includes Chinese herbal medicine, glutathione and new meridian therapy as required. In addition, guidance on diet, exercise and living environment is also provided. New meridian therapy (a type of acupuncture) is an excellent regulator of the autonomic nervous system and improves symptoms by adjusting the parasympathetic dominance of chemical sensitivity (headache, nausea, eye irritation symptoms, choking, dizziness, muscle pain, memory loss, etc.) and returning the autonomic nervous system to an intermediate position between sympathetic and parasympathetic activity. (For more information, see New meridian therapy).