Medical Treatment
MTBI Invisible brain injury due to whiplash
Overview of MTBI
MTBI stands for mild traumatic brain injury. It is referred to as an invisible brain injury. Why is it called invisible? This is due to the fact that it cannot be detected on traditional CT or MRI imaging.
Because MTBI is caused by a "violent shaking impact" of the head like whiplash, which results in microscopic tearing to cranial nerve fibers that can be detected with a microscope (axonal fiber damage), it cannot be visualized with CT or MRI, is considered normal, and is left untreated and without medical care or compensation.
In recent years, imaging techniques have been developed to make these invisible wounds visible: fiber tractography, an MRI-based technique that visualizes brain nerve fibers by imaging the flow of water in nerve bundles, is the most suitable technique for MTBI and can depict the wounds in about 60% of people with MTBI. The others are SPECT and PET, which can depict decreased blood flow in the brain due to MTBI. SPECT is a technique to image cerebral blood flow by injecting a radioisotope that binds to brain tissue. This allows brain damage to be manifested.
Due to the damage to the nerve fibers in the brain, MTBI patients often have disabilities such as forgetting to turn off the gas, forgetting keys or cell phones, difficulty understanding conversations, difficulty with speech, difficulty doing two things at once, and personality changes such as becoming angry.
How MTBI occurs
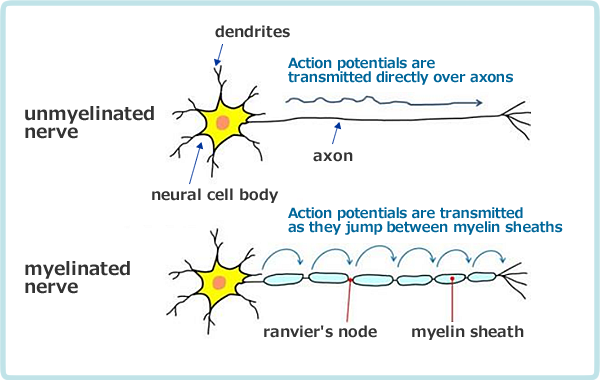
Neurons in the brain are made up of neuronal cell bodies, short dendrites and long axons (axon fiber), from the cell bodies. In MTBI, the axon fibers are mainly damaged. When this occurs extensively, it is called diffuse axonal injury.
This is called an axonal injury. When this occurs over a wide area, it is called a diffuse axonal injury.
(From Clinical Nurse/Medica LBRA)
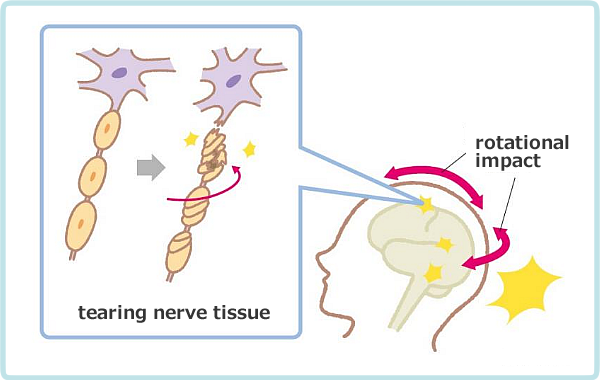
Figure 5-2 shows how axonal damage occurs. As shown, when a rotational impact occurs to the head, such as whiplash, a twisting force acts on the axon, resulting in a tear of the axon. Then, axons drop out, collapse, and nerve cells become inactive and necrotic.
Depending on the location of the lost or disintegrated axons, the patient may experience impaired consciousness, higher brain dysfunction, brain localization functional signs, cranial nerve palsy, motor and sensory palsy in the limbs, cerebellar symptoms, vesico-rectal disorders, and extrapyramidal disorders.
Diagnostic criteria for MTBI
In 1993, the American Association for Rehabilitation Medicine (AARM) first published a definition of MTBI. The key point to be evaluated in this criterion is that loss of consciousness is not an absolute condition, but that MTBI can be diagnosed if the following items are satisfied. The criteria include mild alterations in consciousness, such as fainting, disorientation and clouding of consciousness, traumatic amnesia and focal neurological deficit symptoms.
The diagnostic criteria for MTBI as reported by WHO in 2004 is basically the criteria follow those of AARM.
Frequency of MTBI and sequelae
It has been reported that in the clinical course of Mild TBI, there are 7% to 33% of cases in which symptoms are left behind and do not heal and become chronic. It is estimated that 2% of Americans, or 5.3 million people, are currently living with the sequelae of TBI. A similar high incidence is estimated in our country.
Thus, MTBI is a disease of high frequency of occurrence; the only diseases more frequent than MTBI are migraine headaches and shingles.
Depending on the country, it is estimated that between 100 and 500 cases of MTBI occur per 100,000 population. One report estimates that there are 180 cases of MTBI per 100,000 population, of which 15%, or 27 cases, have prolonged symptoms. This is a very large frequency.
Fiber tractography
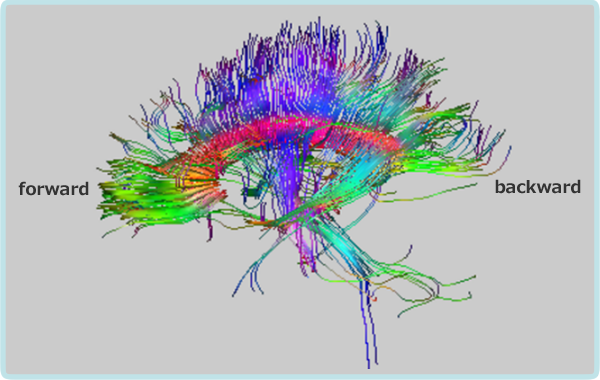
The colors are shown in blue for the vertical direction, green for the anterior-posterior direction, and red for the left-right direction.
Fiber tractography(Hereinafter referred to as FT) in a case of diffuse axonal injury by a traffic accident
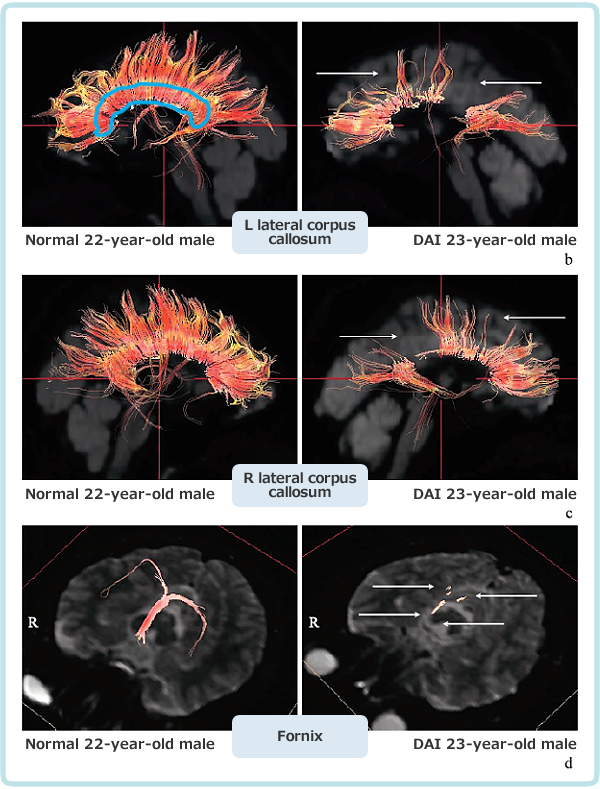
The blue area shows the corpus callosum, and the surrounding area shows the nerve bundles extending from the corpus callosum to the hemispheres.
The upper two rows show the corpus callosum and the lower rows show the fornix. (Ken Sugiyama et al.)
Figure 5-4 shows FT of a case of higher brain dysfunction by a traffic accident (with intellectual, attention, memory and executive function impairments) by Ken Sugiyama et al. In this case, conventional CT/MRI can’t detect any abnormalities, but FT shows more pronounced damage to the corpus callosum and fornix compared to healthy subjects in the left column.
SPECT (cerebral blood flow scintigraphy)
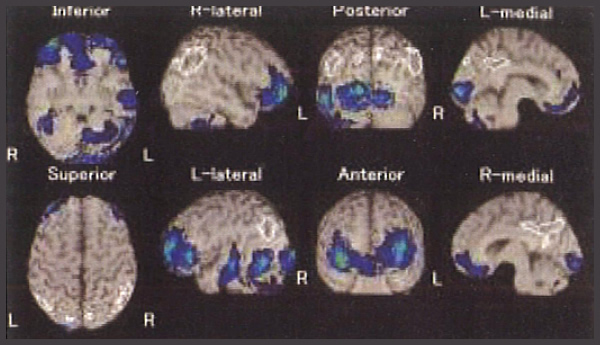
Brain SPECT test stands for single photon emission computed tomography of the brain. A small dose of a fat-soluble radiopharmaceutical that tends to accumulate in the brain is injected. The distribution of radiation (gamma rays) emitted by the drug that accumulates in the brain is photographed by a scintillation camera and displayed as a tomographic image. This detects localized reduced blood flow due to brain damage.
In head trauma, brain SPECT images are useful for understanding the pathophysiology, diagnosis, treatment, prognosis, and efficacy of treatment. SPECT has the advantage that the whole brain can be evaluated and statistical analysis images can be easily generated by comparison with standard databases.
A case of cerebral hypoperfusion on SPECT: 53-year-old male. Two years ago, he suffered loss of consciousness due to traffic trauma and was treated at another hospital as concussion. After returning to work, he showed decreased concentration, memory, and work efficiency. Symptoms such as headache, dizziness, tremor, and numbness also persisted. Brain MRI showed no obvious brain contusion, but white matter lesions in the bilateral frontal subcortex. SPECT showed decreased blood flow in the bilateral frontal lobes, and this finding did not change when examined 2 and 3 years after head injury, indicating irreversible neurological damage. The patient was diagnosed as having higher brain dysfunction. (From Hiroshi Matsuda: The Perfect Guide to Brain SPECT)
Cases of MTBI
The following sections describe cases of MTBI and moderate TBI that we have diagnosed or treated.
Case 1
MTBI, higher brain dysfunction (memory impairment, attention impairment, executive function impairment), balance disorders, depression, and various other disorders.
A 46-year woman. 2-years ago, she was driving on her way to work, when the car in front of her slowed down, the driver of a light truck behind her was picking up a bottle and did not realize she was slowing down and hit her car. Her head and neck were struck several times by the headrest. Immediately afterward, she was in a daze. She visited an orthopedist and was diagnosed with a cervical sprain.
The day after the injury, she was driving when she could no longer read the car's navigation system, got lost on a familiar road and went deep into the mountains. She also got lost the following day. She also went to work the next day, but when she wandered around at work, unable to walk straight, her boss told her to go home. She saw a neurosurgeon and an orthopaedic surgeon again, but nothing changed, and from the next month she visited another hospital, where she was diagnosed with traumatic stress disorder.
2 years after the accident, she visited our clinic for exam. and treatment.
- Initial symptoms
- persistent pain in neck to shoulder and both arms. Headache, insomnia, flashbacks to the accident. She has loss of appetite, weight loss of 8 kg, numbness around her lips, pain, tingling, and tremors in her right hand. She is physically weak, lacks motivation, and has difficulty going out because she does not want to see people. Frequent nightmares. Can’t ride in a car (fear of driving. She rides only as much as necessary). Lacks attention and concentration, forgetfulness. Communication difficulties. Tachycardia due to anxiety when going outside. Inability to open eyelids, pain behind the eyes, and a variety of other symptoms.
- Higher brain function tests
-
Standardized language test Relational pair words 4-4-5(/10) Irrelevant pair words 0-1-1(/10)
Evaluation: memory impairmentRivermead Behavioral Memory Test (Everyday Memory Test) 17 points
Evaluation: mild memory impairmentRey-Osterrieth Complexed Figure test(ROCF)(visual memory test) Immediate replay 12 points
Evaluation: AbnormalZung test Moderate depression The patient needs some assistance in all daily living skills. Communication, problem solving, persistence and endurance, and social skills require some or considerable assistance. The condition is equivalent to some loss or considerable loss.
- FT findings
-
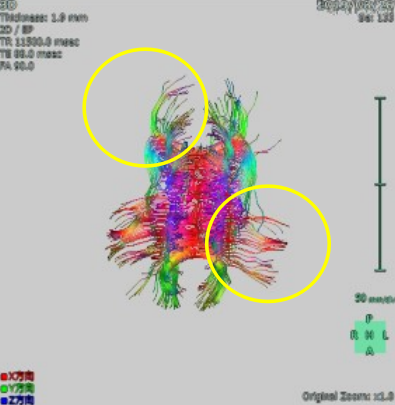
Figure 5-6: Axonal fiber reduction in the left central part of the corpus callosum and right greater forceps. 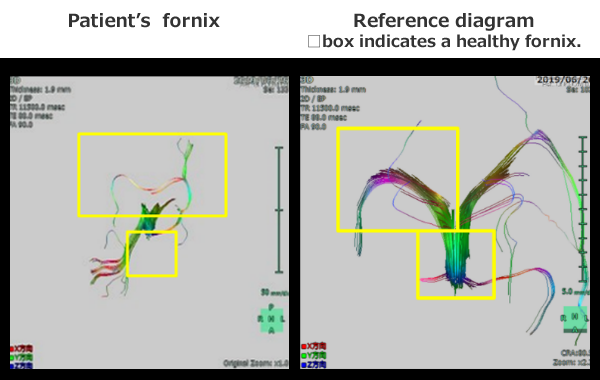
Figure 5-7. Fornix: the crus and the body of fornix are missing.
The □ boxes in the right diagram show the normal crus and body of fornix.Figures 5-6, 5-7 show FTs of the individual. There is a decrease in axonal fibers in the left central part of the corpus callosum and in the right large forceps. The crus and body of the fornix are also observed to be deficient. The right large forceps shows a decrease in axonal fibers to the occipital lobe related to vision, reflecting the loss of visual function due to the car accident. The prominent loss of the fornix is associated with memory impairment due to the accident.
- Opinion of a neurosurgeon from the Bureau of Labour Standards on workers' compensation
-
The following opinion was submitted by the Bureau's physician. “The conventional imaging diagnosis had difficulty in seeing the abnormal area of MTBI. In this case, diffusion tensor imaging (Fiber tractography) showed a decrease in axonal fibers in the left central part of the corpus callosum, a decrease in axonal fibers in the right occipital region, and a decrease in axonal fibers in the left right fornix. I consider these findings to be those of MTBI."
With this opinion, the patient's MTBI was certified. The abnormal findings of fiber tractography were adopted in that case.
- Treatment Progress
-
Initial symptoms have been reduced by half due to the new meridian therapy. She has persistent pain in the back of her neck, decreased sense of taste, and can recognize stimulants such as curry and kimchi, but other foods are difficult to recognize. Attention and concentration have improved with new meridian therapy. She no longer forgets to turn off the gas or electricity, which was initially the case. Initially, she was unable to cook two dishes at the same time, but with some ingenuity, she is now able to do so. Initially, she did not drive a motor vehicle, but she can now drive for 15 minutes. She dreams, but no longer has nightmares. Communication was initially sluggish after 10 minutes of talking on the phone, but has improved to the point where she can now talk for more than an hour.
Thus, the new meridian therapy is effective for MTBI and can improve higher brain dysfunction by improving blood flow to the brain.
Case 2
A case with abnormalities on SPECT
-
Female, in her 20s
TBI (traumatic brain injury), higher brain dysfunction (memory impairment, attention/concentration disorder, executive dysfunction, social behavior disorder)This case patient was hit by a car 9 years ago and suffered a brain contusion in the orbitofrontal region. After the accident, her personality changed and she became obsessive and angry easily. And she has a strong symptoms of memory loss and tiredness. There are obstacles in relationships at work. She cannot remember new things and has to make notes of everything. Because of these impairments, she is greatly hindered at work.
- SPECT examination revealed the following abnormalities.
- (1) The overall cerebral blood flow is considerably reduced to less than 30 ml/100g/min.
(2) Blood flow reduction was depicted in the basal portions of the bilateral frontal lobes and the left limbic region of the occipital lobe, and it was pointed out that these changes were caused by brain damage. (See Figure 5-8)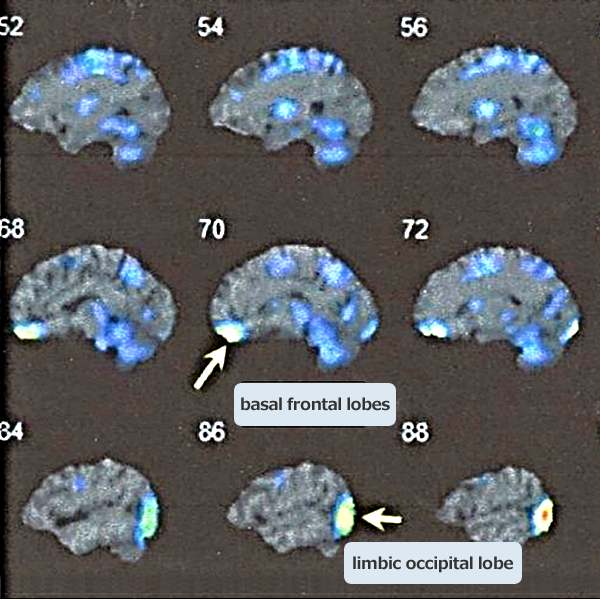
Figure 5-8. 3D-SSP shows hypoperfusion in the bilateral basal frontal lobes and the left limbic occipital lobe (arrows).
White areas indicate areas with strong cerebral hypoperfusion on SPECT.Cerebral blood flow indicates the average blood flow ml per minute per 100 g of brain tissue. The lower limit for the entire normal group (<5% occurrence) is 31.0 ml/100 g/min, and this patient's cerebral blood flow is below this limit. In the 20s, it is around 46 ml, which is clearly below this level.
- Summary
-
1) Overall cerebral blood flow is considerably reduced. This finding indicates decreased cerebral blood flow and brain function due to diffuse axonal damage throughout the brain caused by brain injury TBI.
2) Locally, decreased blood flow is seen in the basal areas of the bilateral frontal lobes and in the limbic area of the left occipital lobe.